How should we measure our impact?

Cecilia Tilli, Secretary-General of the Foundation to Prevent Antibiotic Resistance
The Foundation to Prevent Antibiotic Resistance has joined the Swedish impact measurement network Effektfullt, a partner network of Social Value International. We will work together with other change-making organizations to develop effective ways to measure our impact.
For any organization striving to achieve change, impact measurement is essential. If we do not know the impact our efforts have, we do not know if we are spending our resources well. A for-profit organization needs to know if it is profitable – a for-impact organization needs to know if it is impactful.
However, measuring impact is much less straightforward than measuring profit. To start with, it is often far from obvious which units should be used. If we want to be able to compare very different interventions, it would be good to use something general – for example “lives saved” or QALYs. In practise, however, this is often very difficult to measure or even estimate for specific interventions. Instead, one might go for more specific measurements. An organization working to improve education might measure what fraction of students graduate; an organization promoting green energy might measure their impact in estimated CO2 savings.
The goal of our foundation is to prevent antibiotic resistance. We aim to protect the modern healthcare that heavily depends on effective infection treatment. “Protecting modern healthcare” may sound abstract, but the fact is that virtually everybody today has antibiotics to thank for ensuring the health or life of a loved one. Effective antibiotics is what makes complicated surgeries possible and routine surgeries safe; they enable chemotherapy treatments as well as treatment for pneumonia and urinary tract infections. Now, resistance to antibiotics is increasing and threatens to cause millions of deaths per year.
“Protecting modern healthcare” may sound abstract, but the fact is that virtually everybody today has antibiotics to thank for ensuring the health or life of a loved one.
So how do we prevent this from happening?
To prevent antibiotic resistance, we need to understand and address the drivers of this complex issue. For example, one driver of resistance is the use of antibiotics for viral infections (where antibiotics have no positive effect) or for minor bacterial infections (where antibiotic use is unnecessary). This is a kind of misuse of antibiotics, typically driven by poor prescription practices. Maybe there are no good guidelines in place, or maybe the antibiotics are sold over the counter directly to the patient without a prescription. Sometimes, the resources for a proper diagnose is lacking – which in turn could be a result of poverty or of policy decisions. Sometimes, even though proper guidelines and routines are in place, the patient themselves push hard for antibiotic treatment because they believe that is what they need.
If we want to address resistance driven by these kinds of misuse, there are many possible options. The most apparent ones might be to work for improved prescription guidelines and regulations, but we could also try to address the underlying causes such as access to diagnostics, improving relevant policies or educating the public about the harm done by misuse of antibiotics. We could also work on the drivers of infection – if people became healthier in general, antibiotic consumption would be reduced both for justified treatments and for misuse. Or we could develop and promote alternative treatments, that might reduce the demand for antibiotics.
Impact measurement will always be a challenge, especially for complex and difficult problems, but it is also key to developing interventions that work.
The strategies above are only a few illustrative examples out of many and mapping out this complex web of drivers is an important task to be able to formulate plausible prevention strategies. When we know what the drivers are, we can choose strategically which ones to target – where we believe our interventions can make the greatest difference. However, without impact measurement we would never know if we got it right. Did the information campaign actually lead to higher awareness and better patient behaviour? Was the health promoting intervention successful in decreasing infections in the target group? Did development of alternative treatments offset antibiotic use in a way that reduced resistance development?
Impact measurement will always be a challenge, especially for complex and difficult problems, but it is also key to developing and improving interventions that work. We are not the first or the only ones to tackle difficult problems. Working together with other members of Effektfullt we will be able to continually build and improve our impact measurement strategies.
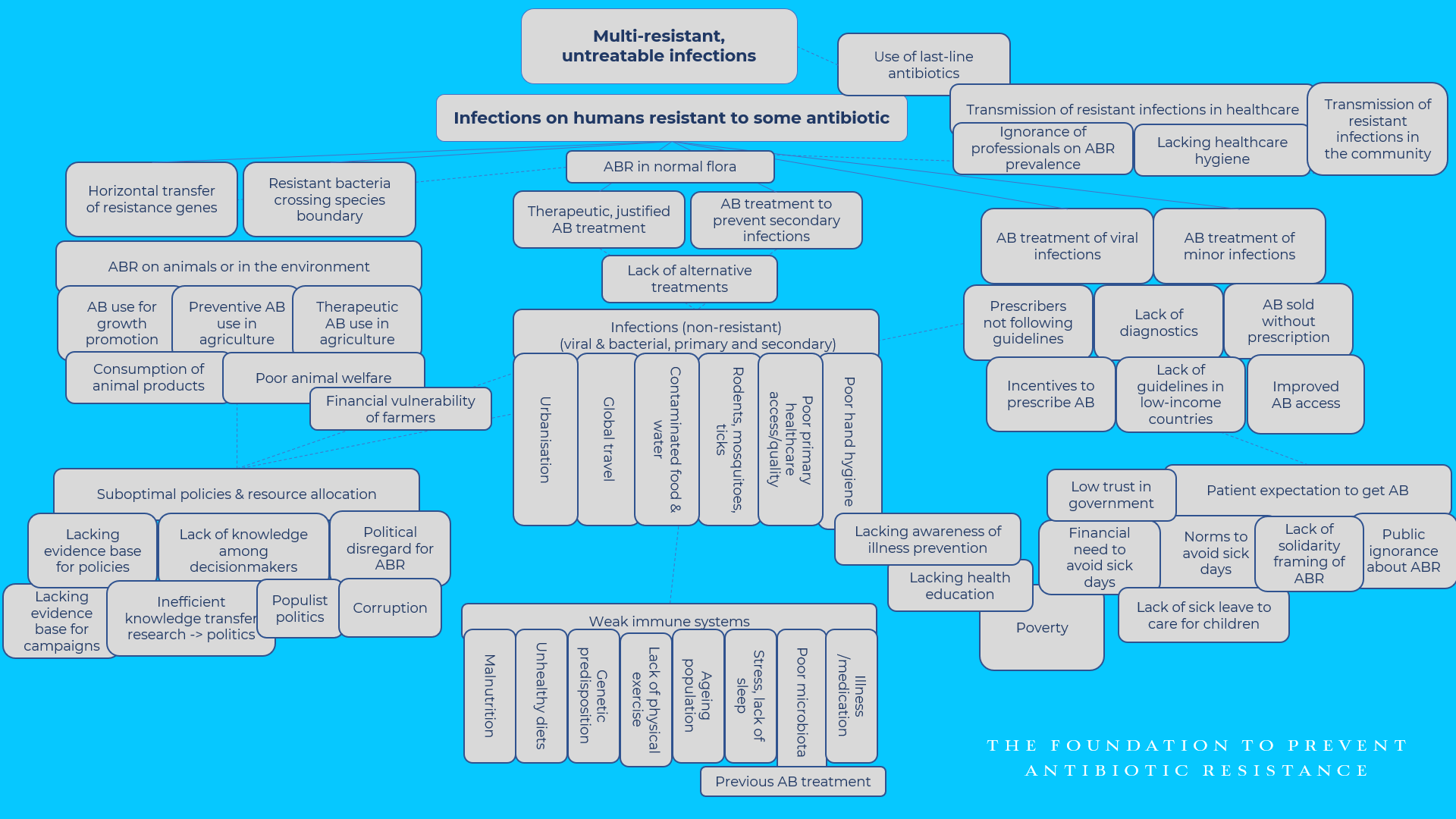
Tentative mapping of drivers of antibiotic resistance. © The Foundation to Prevent Antibiotic Resistance
Related articles
New collaboration between PAR Foundation and the Global AMR R&D Hub
– The collaboration with PAR Foundation is an excellent example for how the Dynamic Dashboard and the work of the Global AMR R&D Hub can support funders and stakeholders in the AMR R&D field more broadly, says Dr Elmar Nimmesgern, who leads the work of the Global AMR R&D Hub from their offices in Germany.
Opinion: Resistance could pose the greatest threat to our health
Debate article by The Foundation to Prevent Antibiotic Resistance, published in one of Sweden’s major daily newspapers Svenska Dagbladet 18 November 2020.
Antibiotic resistance and Sustainable Development Goals
The Sustainable Development Goals (SDG’s) guide investment in sustainable development, and the lack of inclusion of antibiotic resistance has therefore been problematic. The recent review has added one indicator of resistant infections, but most of the links between resistance and the SDG’s are still implicit. Even so, rising awareness of the importance and fragility of global health can hopefully pave way for a greater recognition of the intimate connections between antibiotic resistance and sustainable development.