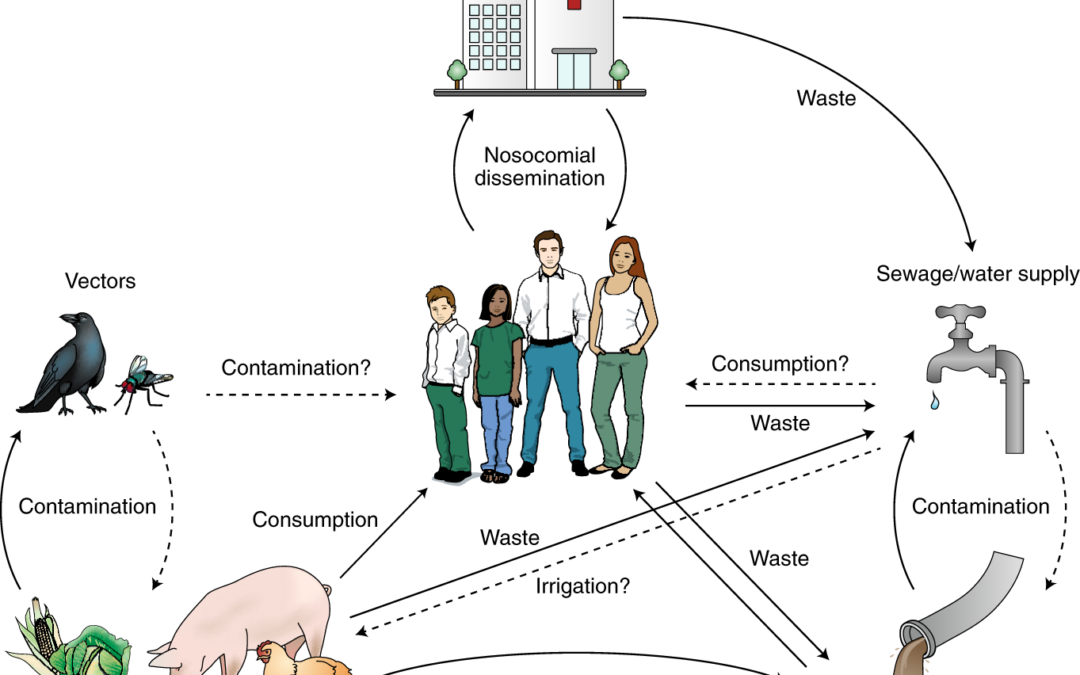
A one-health approach to antimicrobial resistance. Image Credit: Nature
Antimicrobial resistance remains a global health challenge, not just for humans, but also for animals and the environment. Antimicrobial resistance occurs when pathogens develop immunity to antibiotic drugs. With the use of antimicrobials in agriculture, veterinary medicine, and human medicine in modern times, it is high time every stakeholder concerned about AMR contributed to using a One-health approach.
This bacterial immunity happens through a number of mechanisms. For example, the transfer of genes from resistant microorganisms to other microorganisms. Antimicrobial-resistant microorganisms proliferate and pass on their traits very quickly. This makes them capable of invading entire populations and causing epidemics.
Many times, a resistant pathogen that infects humans has its origins in lower animals or even plants. Diseases caused by such organisms are called zoonoses and phytonoses, respectively. These infections happen because of the interaction between man, animals, plants, and the environment.
Zoonotic and phytonotic infections are huge contributors to antimicrobial resistance. This is because antimicrobials that treat human infections are also used to treat animal infections. For instance, the use of fluoroquinolones in treating urinary tract infections (UTI) in humans and domestic animals like dogs and cats.
Also, animals resistant to fluoroquinolones can transmit resistant bacteria to humans. Even when combating AMR in human populations, there is a risk of resistance already started in animal populations before being transmitted to humans.
Studies have also shown that antimicrobial-resistant organisms reside in the soil, water, and air where antimicrobials are used. Sewage, manure, and pharmaceutical industry waste pollute the environment and deposit these organisms into the ecosystem. The environment then becomes a reservoir for resistant microorganisms. This interaction between humans, animals, and the environment is inevitable. Hence, the need to combat AMR infections on all fronts.
One health approach
The One Health approach is a proven solution to fighting the AMR pandemic on all fronts. This approach recognises the interactions that occur between animals, humans, and their environment, and emphasises the need for a strategy that works across these sectors. For example, evidence shows that the indiscriminate use of fluoroquinolones in veterinary medicine leads to quinolone resistance in Salmonella spp. strains that infect the human gut. It is evident that the suboptimal use of antibiotics in one discipline can cause the incidence of antimicrobial resistance in another.
The One Health approach encourages all sectors of health to become responsible and aware of how they contribute to the spread of antimicrobial resistance. To achieve this, the one health approach specifies the best means to use antimicrobials across the health, agricultural and environmental disciplines to ensure a better outcome.
As part of the One Health Approach, the World Health Organization (WHO) has developed five (5) main pillars to help combat antimicrobial resistance.
The first pillar focuses on improving public awareness about antimicrobial resistance. AMR develops due to the overuse and underuse of antimicrobials. In rural areas, where people cannot afford a diagnostic test, over-the-counter purchases of antibiotics and antimalarial drugs are very common.
- Many agriculturists make use of antimicrobial drugs indiscriminately, such as the use of the antibiotic Colistin as a growth promoter in domestic animals. To tackle this, the One Health approach creates awareness through public campaigns to educate people on the dangers of antimicrobial misuse. It also teaches people how to use antimicrobials only when necessary.
- The next pillar is the need to strengthen global surveillance and further research into antimicrobial resistance. Efforts to combat AMR should also target monitoring AMR rates in samples from humans and the environment, and also ensure that health professionals practise the safe use of antimicrobials and map out more innovative approaches to combating the spread of antimicrobial-resistant microorganisms.
- Another pillar emphasises the use of preventive measures. Individuals living in overcrowded regions and people with poor nutrition are most susceptible to antimicrobial resistance. The use of proper sanitation and healthy living in susceptible regions can benefit animals, humans, and the environment.
- The fourth pillar discourages the use of antibiotics as prophylactics or growth promoters, or for any other non-therapeutic use. It is imperative that antibiotics be administered at optimal doses. This ensures that bacteria and other microorganisms are completely eliminated, with little to no risk of becoming resistant.
- The last pillar is an economic approach that focuses on creating an enabling environment to combat the spread of antimicrobial resistance. There is an urgent need to adequately invest in research and development efforts to produce more effective drugs and vaccines. This will improve on early detection of AMR, and also support other interventions to combat the spread of antimicrobial-resistant infections.
The adoption of the one health approach offers a comprehensive strategy to address the challenge of antimicrobial resistance in modern society. By fostering cooperation across sectors, this approach empowers us to regulate the use of antimicrobials and mitigate the emergence of new resistant strains. To effectively combat antimicrobial resistance, it is crucial that all stakeholders prioritize the judicious use of antibiotics. The one health approach facilitates such collective action and provides a viable path towards achieving our goal.